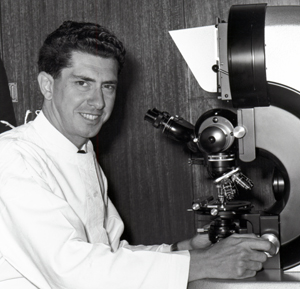
Communications Adviser Leigh Dayton talks to Cartherics Scientific Board member Jacques Miller – the man who discovered the function of the thymus gland yet didn’t win the Nobel Prize.
 |
 |
IMMUNOLOGIST Jacques Miller did not win this year’s Nobel Prize in Physiology or Medicine. He didn’t win it last year or the year before that. In fact, the French-born Australian has never won the prize.
“For more than four decades, people officially invited by the Nobel Committee to select potential awardees have told me that they had nominated me,” says Miller, a member of Cartherics’ Scientific Advisory Board and Emeritus Professor at the Walter & Eliza Hall of Medical Research.
“I hope I have not disappointed them or let them down by not getting this award,” quips the scientist who in 1961 discovered the immunological function of the thymus and who in 1967 identified the existence of the two major types of lymphocytes, T cells and B cells.
Far from disappointing his colleagues, Miller – widely considered to be the single living individual most deserving of a Nobel prize who has not been awarded one – conducted work which underpins key medical advances, from vaccinations to cell, tissue and organ transplants. In fact, the field of immunotherapy and its CAR-T centre piece is fundamentally dependant on the research empire his findings created.
Better still, Miller continues to explore the world of the immune system.
Communications Adviser Leigh Dayton talked with Jacques Miller about how immunology has developed since those heady days in the 1960s.
LEIGH: First of all, how did you come to study immunology and the thymus gland as a young scientist?
JACQUES: In 1958, after my internship at the Royal Prince Alfred Hospital in Sydney I got a Fellowship to study cancer research at the Institute for Cancer Research in London. For my PhD, I chose to work on mouse lymphocytic leukemia, a cancer induced by giving a virus during the immediate newborn period but not later. It arose in the thymus and spread to other tissues at around 2 months of age.
I surgically removed the thymus (thymectomy) at around 6 weeks of age and none of these mice ever became sick in any way. Grafting a one-day-old thymus as late as 6 months after adult thymectomy restored the potential for leukemia development. I reasoned that the virus had to be given at birth because it might be able to multiply only in certain cells that were present in the one-day old thymus before spilling over to the rest of the body. If this were so, removing the thymus at birth before injecting the virus, and grafting a one-day-old thymus 2-6 months later should not be associated with leukaemia development.
The mice thymectomized at birth, however, became sick and wasted unlike any of the mice thymectomized as adults. They had far fewer white blood cells (lymphocytes) than normal mice and were unable to reject foreign skin grafts. This was a eureka moment! It became evident that the thymus in early life was responsible for providing the body with the cells responsible for defence mechanisms. These findings, first obtained in 1961, opened up the whole field of immunology.
LEIGH: And then you identified T cells and B cells.
JACQUES: Yes. In 1966-1968, together with my first PhD student, Graham Mitchell, we cannulated the main lymphatic duct of immunocompromised thymectomized mice and normal mice to get a quantitative measure of their lymphocyte and immune defects. As some of these mice had been irradiated we had to protect them from irradiation damage with a source of stem cells which was bone marrow. The stem cells restore blood forming cells like red blood cells.
Experiments with such mice, following an injection of sheep red blood cells (SRBC), showed clearly that the mice had two major types of lymphocytes responding to the SRBC: one was derived from the thymus (now called T cell) but not forming antibody, the other derived from bone marrow (now called B cell) and responsible for producing antibody, though in most cases requiring help from T cells to do so. This was another eureka moment.
LEIGH: What do you see as the key advances in immunology since your discoveries?
JACQUES: There have been many key advances since my discoveries and these have been due mostly to our increasing knowledge of molecular biology and genomics. To just name one, I would single out the intricate work done by Ian Frazer that resulted in a highly successful vaccine against human papilloma virus, a causative agent of cancer in humans.
LEIGH: What is the future of immunology?
JACQUES: T cells appear to be involved essentially across the entire spectrum of tissue physiology and pathology, not just in reactions or diseases considered to be bona fide immunological such as autoimmunity or immune deficiency, but also, for example, in tissue repair, gastro-intestinal aberrations, pregnancy pre-eclampsia, and in many types of cancer.
New technology and approaches, now becoming available, will lead to a much deeper understanding of many of these conditions. They also promise safer alternatives to existing treatments such as chemotherapy and radiation. The ‘off-the-shelf’ therapies Cartherics is developing are a case in point.
Hence the thymus and its cells will occupy researchers and clinicians for decades to come. That organ — previously stated to be useless and populated by cells which in 1963 were considered by Nobel Laureate Peter Medawar to be “an evolutionary accident of no very great significance” — has certainly come of age!


